At New-York Presbyterian/Weill Cornell Medicine, endocrine surgeons are conducting novel research that brings new insights into pediatric papillary thyroid carcinoma (PTC), the most common form of differentiated thyroid carcinoma (DTC) in children. While pediatric PTC has distinct clinical and pathological differences compared to adult PTC, little is known about the dynamic interplay between age and the risk of advanced disease in the pediatric population.
This sparsity of knowledge propelled Brendan Finnerty, MD, FACS, Director of Interventional Endocrine Surgery, and others at NewYork-Presbyterian/Weill Cornell Medicine to conduct a large cohort study that examined the connection between PTC and age in the pediatric population compared to a young adult population. Their discovery -- that prepubertal children are more likely to have more advanced disease at diagnosis than are adolescents or young adults -- underscores the importance of age as a key consideration in treatment approaches to pediatric PTC and identifies important future research directions to improve outcomes.
“The impetus for this study is we’re always seeing patients in the clinic who present with scenarios in which there's a gap of knowledge in the literature,” explains Dr. Finnerty, a surgeon with expertise in endocrine and neuroendocrine surgical oncology. “For instance, we really don’t know the true clinicopathologic features of PTC tumors dependent on age in children. This is because no large, contemporary cohort study has ever been conducted to determine whether younger children are at higher risk for advanced PTC at presentation compared to adolescents.”
No large, contemporary cohort study has ever been conducted to determine whether younger children are at higher risk for advanced PTC at presentation compared to adolescents.
— Dr. Brendan Finnerty
Optimal management of PTC needed based on patient age
PTC is the most common form of differentiated thyroid carcinoma (DTC), a group of thyroid cancers that also includes follicular thyroid cancer. Although pediatric DTC only accounts for 1% of all pediatric cancer cases in prepubertal children, the incidence rises to 7% in adolescent cancer cases. Pediatric PTC typically presents as a solitary nodule, tends to grow slowly, and often spreads to the lymph nodes in the neck. At diagnosis, up to 40-60% of children with PTC will have thyroid cancer that has spread to the lymph nodes in the neck, and approximately 10-15% of patients with lymph node metastases will have thyroid cancer that has spread to the lungs.
“Our study sought to further understand the relationship between age and progressive PTC to improve the management of pediatric patients,” he explains. “Although pediatric PTC is highly treatable, the incidence is slowly rising, so our goal to stay ahead of the curve with insights and treatment strategies that eradicate cancer with the fewest complications possible.”
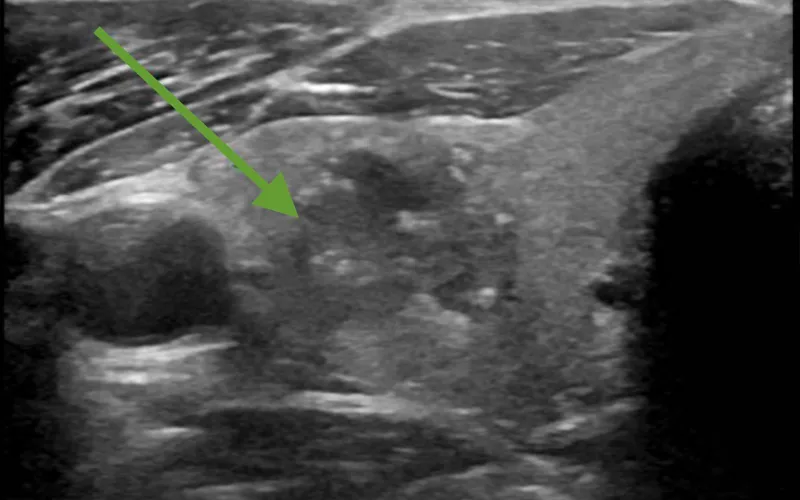
Neck ultrasound detection of right-sided thyroid cancer
For the majority of children and adolescents, PTC is highly treatable and the prognosis is usually excellent. Treatment typically consists of a total thyroidectomy and surgical resection of any involved lymph nodes. However, says Dr. Finnerty, many open questions remain regarding the optimal management of PTC in young versus older children.
In 2015, the American Thyroid Association (ATA) published its first set of guidelines for pediatric PTC. “When the guidelines were written, the ATA stated that it was unclear whether younger patients are at higher risk for PTC,” explains Dr. Finnerty. “I believe the conclusion was based on a 2006 Belarusian study of 800 pediatric patients with PTC that found that younger age was associated with recurrent nodal disease and pulmonary metastasis. The limitation with this study is that most of these children were exposed to radiation as a consequence of the Chernobyl nuclear disaster, so a significant proportion of these patients underwent ionizing radiation to the head and neck before diagnosis.”
After the Belarusian study, smaller studies found younger children with PTC tumors are at risk for a more aggressive disease course, but the relationship between age and tumor aggressiveness remained unclear.
“Our study sought to further understand the relationship between age and progressive PTC to improve the management of pediatric patients,” he explains. “Although pediatric PTC is highly treatable, the incidence is slowly rising, so our goal to stay ahead of the curve with insights and treatment strategies that eradicate cancer with the fewest complications possible.”
Our study sought to further understand the relationship between age and progressive PTC to improve the management of pediatric patients. Although pediatric PTC is highly treatable, the incidence is slowly rising, so our goal to stay ahead of the curve with insights and treatment strategies that eradicate cancer with the fewest complications possible.
— Dr. Brendan Finnerty
Investigating the connection between age and disease progression
For this study, the physicians drew data from the National Cancer Database for pediatric patients ages 18 and younger and young adults ages 19 to 39 who were diagnosed with PTC between 2004 and 2017. Pediatric patients were categorized as prepubertal if they were ages 10 or younger, and adolescent if they were ages 11 to 18. A total of 4,860 pediatric (prepubertal n = 274, adolescents n = 4586) and 101,159 young adult patients were included in the study. Patient demographics, cancer staging, treatment, and overall survival were compared between the prepubertal, adolescent and young adult groups. Tumor characteristics, lymphovascular invasion, treatment methods, and outcomes were also compared.
The study found that prepubertal patients presented with more advanced disease than adolescents and young adults, with significantly larger primary tumors greater than 4 cm (26% vs. 13.5% and 8.3%, respectively). Prepubertal patients had more spread to lymph nodes compared to adolescents (58% vs. 36%) and more extrathyroidal extension (ETE) compared to adolescents (47% vs. 25%). Although there was no difference in the frequency of multifocal tumors between prepubertal and adolescent children (37.2% vs. 35.5%), young adult patients presented with multifocal tumors more frequently than either pediatric group (38.8%). Regarding lymph node invasion, prepubertal patients had more spread to lymph nodes in the neck compared to adolescents and adults (67% vs. 52% and 32%, respectively) and more spread outside of the neck compared to adolescents and adults (11.3% vs. 2.2% and 0.5%, respectively).
Using multivariable logistic regression modeling for the independent predictors of metastases, the team determined that age 10 or younger years old is an independent predictor for high regional disease burden and distant metastases at the time of presentation, even for those with small primary tumors. Additionally, prepubertal age independently predicted lymph node metastases for microcarcinomas. Prepubertal versus adolescent patient age was associated with ETE, even with very small (≤1 cm) primary tumors.
“This study is notable because it captures 70% of all pediatric thyroid cancer diagnoses in the United States, and it is one of the few that had the reference point of a control group of a young adult population, which gives us a landscape of interpretation,” says Dr. Finnerty. “Our findings clarified that there is a spectrum of disease severity for pediatric PTC, starting with a more aggressive phenotype in prepubertal children to a lesser aggressive phenotype in adolescent children, and then to an even lesser aggressive phenotype in a young adult population.”
This study is notable because it captures 70% of all pediatric thyroid cancer diagnoses in the United States, and it is one of the few that had the reference point of a control group of a young adult population, which gives us a landscape of interpretation. Our findings clarified that there is a spectrum of disease severity for pediatric PTC, starting with a more aggressive phenotype in prepubertal children to a lesser aggressive phenotype in adolescent children, and then to an even lesser aggressive phenotype in a young adult population.
— Dr. Brendan Finnerty
“Another nuance of the study is that even if the primary tumor was small (less than 1 cm) in the prepubertal cohort, the level of tumor aggressiveness still remains significant,” adds Dr. Finnerty. “This means even for the smallest tumors we should have a high index of suspicion for more aggressive disease.”
Regarding treatment, most pediatric patients in all of the age groups underwent a total thyroidectomy, although 7.2% of adolescents had a hemithyroidectomy compared with 4% of prepubertal children. Prophylactic lymphadenectomy was more frequent in young adults (50%) versus adolescents (30%) and prepubertal children (18%). Most pediatric patients received radioactive iodine therapy (63% of prepubertal and 59% of adolescents) as compared with 50% of young adults. Five-year survival did not differ between the age groups, with all three reporting a survival rate of higher than 99%.
“Our study data continues to support performing a total thyroidectomy in prepubertal children,” says Dr. Finnerty. “For these children, we still want to be fairly aggressive in our treatment approach by taking out the whole thyroid, because there's a higher likelihood of more aggressive cancer. However, in the adolescent population, there may be patient-specific factors that we can identify in the future that will help us apply a de-escalation approach for patients who may not need a total thyroidectomy.”
With its large sample size and statistical power, this study builds upon the knowledge base for pediatric PTC and provides a platform for more granular studies in the future. “Although the study provided meaningful insights, its limitations include the lack of recurrence rates or tumor genomics data to supplement our findings,” says Dr. Finnerty. “At Weill Cornell Medicine, we routinely use next-generation sequencing assays to assess the genomic profiles of thyroid tumors. Incorporating genomic profile data into a large-scale study would greatly enhance our ability to assess recurrence risk in children with these cancers.”
With its large sample size and statistical power, this study builds upon the knowledge base for pediatric PTC and provides a platform for more granular studies in the future. “Although the study provided meaningful insights, its limitations include the lack of recurrence rates or tumor genomics data to supplement our findings,” says Dr. Finnerty. “At Weill Cornell Medicine, we routinely use next-generation sequencing assays to assess the genomic profiles of thyroid tumors. Incorporating genomic profile data into a large-scale study would greatly enhance our ability to assess recurrence risk in children with these cancers.”
For Dr. Finnerty, NewYork-Presbyterian/Weill Cornell Medicine is the ideal setting to pursue research that would improve the management of children with PTC. “Looking toward the future, our main research questions are, can we deescalate the extent of thyroid surgery in an identifiable set of low-risk patients with PTC, and how can we incorporate tumor genomic factors into risk assessment to guide decision making, perhaps even preoperatively? Those are the future studies that I think are very much warranted.”
Looking toward the future, our main research questions are, can we deescalate the extent of thyroid surgery in an identifiable set of low-risk patients with PTC, and how can we incorporate tumor genomic factors into risk assessment to guide decision making, perhaps even preoperatively? Those are the future studies that I think are very much warranted.
— Dr. Brendan Finnerty
“Here at NewYork-Presbyterian, we have a great group of multidisciplinary physicians and providers that keep lines of communication open to manage these complex patients,” continues Dr. Finnerty. “We’re on the forefront of investigative research to improve diagnostics and treatment modalities for pediatric PTC, and we are integrating our translational research laboratory with clinical care to advocate for our patients' best management options.”



